Our Blog
12 Steps to Early Diagnosing Hepatic Cystic Lesions
April 26, 2025
Early diagnosis of hepatic cystic lesions can make a significant difference in patient outcomes. In this article, we’ll explore twelve comprehensive steps that healthcare providers can take to ensure accurate and timely diagnosis. With a friendly and straightforward approach, we’ll break down the diagnostic journey, empowering you to understand this important health topic.
1. Understanding Hepatic Cystic Lesions
Start with a clear definition of hepatic cystic lesions to provide a foundation for understanding their significance and implications. Hepatic cystic lesions are fluid-filled sacs that develop in the liver, typically benign, though they can sometimes cause symptoms if they grow large enough. Recognizing what these lesions are helps patients and healthcare providers understand the importance of monitoring and diagnostic measures.
In this section, it’s crucial to highlight the types of cystic lesions that can occur, such as simple cysts, complex cysts, and even hydatid cysts. Each type carries its own set of implications for diagnosis and management. People often associate these lesions with serious conditions, but many are harmless and found incidentally during imaging for other reasons. This understanding can ease anxiety and encourage proactive healthcare decision-making.
2. Identifying Symptoms and Signs
Recognizing the symptoms associated with hepatic cystic lesions can help initiate the diagnostic process. While many patients remain asymptomatic, others may experience abdominal pain, discomfort, or even bloating. It’s vital to alert patients about these signs, emphasizing that awareness can lead to early medical consultations.
Additionally, some patients may experience complications if the cysts grow, such as infection or rupture. Symptoms can then become more pronounced, such as fever or jaundice. Therefore, healthcare professionals must educate their patients about these potential developments, ensuring they understand the importance of seeking medical advice when these symptoms arise.
3. Taking a Detailed Medical History
Gathering comprehensive medical history is crucial in identifying potential risk factors related to hepatic cystic lesions. A focused history can reveal whether a patient has conditions that predispose them to liver issues, such as liver cirrhosis or previous liver surgeries. This information is essential for a tailored diagnostic approach.
Furthermore, understanding family history plays a significant role. Genetic predispositions to certain liver conditions can influence the likelihood of developing hepatic cystic lesions. Engaging patients in discussions about their family’s health history promotes a well-rounded strategy in evaluating risk factors.
4. Performing a Physical Examination
A thorough physical examination can reveal important clues about the presence of hepatic cystic lesions. Palpating the abdomen may uncover any abnormalities, such as tenderness or enlargement of the liver or gallbladder. During the examination, healthcare providers should remain attentive to any unusual findings that might prompt further investigation.
Additionally, observing other systemic signs like jaundice or swelling in the lower extremities can provide valuable diagnostic insights. A systematic approach during the physical exam creates a robust foundation for subsequent investigative steps.
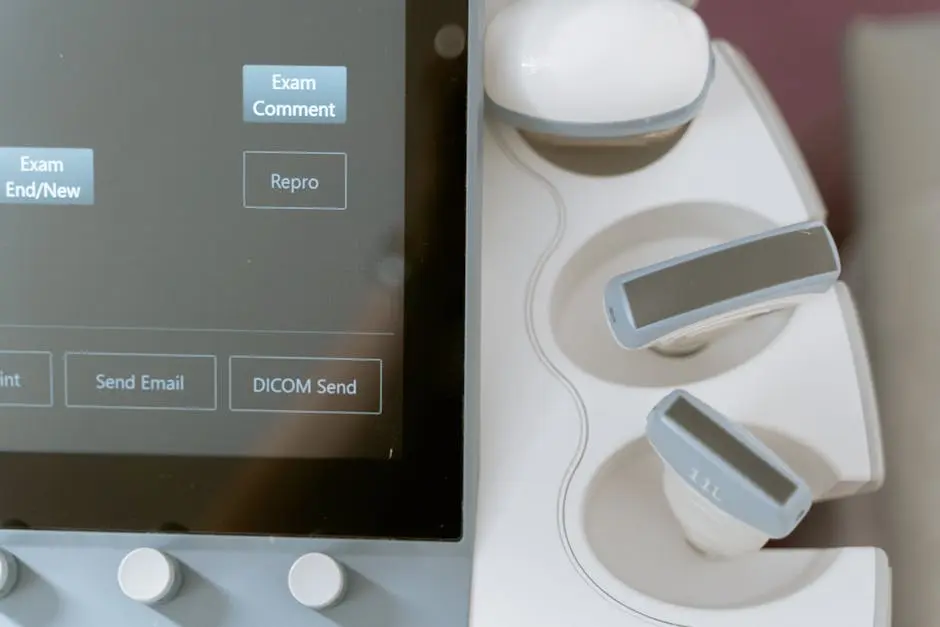
5. Utilizing Imaging Techniques
Different imaging modalities provide invaluable information, helping to visualize the lesions accurately. Ultrasound is often the first-line imaging technique due to its accessibility and safety. It allows for the quick identification of cystic lesions without exposing patients to radiation.
In cases where ultrasound findings are inconclusive, CT scans or MRIs can offer a more detailed view. These advanced imaging techniques can distinguish between different types of cysts and other intra-abdominal pathology, aiding in establishing an accurate diagnosis.
Moreover, it’s essential to consider how often imaging should be repeated based on the nature of the lesions. Monitoring changes over time can help determine if a cyst is benign or requires further intervention.
6. Ordering Laboratory Tests
Lab tests can assist in assessing liver function and detecting abnormalities that may suggest cystic lesions. Basic liver function tests provide essential insights into a patient’s liver health, enabling timely interventions when needed.
Additionally, specific tests like alpha-fetoprotein (AFP) tests can help detect hepatocellular carcinoma, particularly in patients with established liver disease. Tailoring laboratory tests to the patient’s history and imaging findings plays a key role in guiding proper diagnosis and treatment.
7. Differentiating Between Types of Cysts
Understanding the differences between various types of hepatic cysts is essential for accurate diagnosis. Simple cysts are typically asymptomatic, while complex cysts may warrant further investigation due to their potential to harbor malignancy.
Healthcare providers must use imaging and laboratory data to classify cysts appropriately, emphasizing the importance of this step in treatment planning. Correctly identifying the type of cyst can guide decisions about surveillance or intervention strategies.
8. Consulting with a Specialist
Involving specialists can provide further insights and confirm diagnostic findings related to hepatic cystic lesions. Referrals to gastroenterologists or hepatologists offer access to advanced knowledge and tools that can enhance patient care.
Having a multi-disciplinary team approach ensures that all aspects of a patient’s health are considered when managing hepatic cystic lesions. This collaborative effort promotes a thorough evaluation, ultimately leading to better patient outcomes.
9. Creating a Differential Diagnosis
Developing a differential diagnosis helps in ruling out other conditions that may mimic hepatic cystic lesions. It’s important to consider various entities, such as abscesses or tumors, and how their presentations differ from benign cysts.
A thorough differential diagnosis not only aids in accurate identification but also ensures that unnecessary treatments are avoided. Always remain vigilant to the possibility of overlapping symptoms, and use all available information to guide clinical decision-making.
10. Utilizing Follow-Up Imaging
Follow-up imaging is vital in monitoring any changes in cystic lesions over time to guide treatment. Regular imaging can identify trends in lesion size or characteristics, indicating whether the cyst is behaving benignly or requires further action.
Moreover, follow-up imaging also reassures both the healthcare provider and the patient. Knowing that lesions are stable can significantly reduce anxiety and contribute to an overall sense of wellbeing.
11. Implementing a Management Plan
Having a clear management plan ensures that appropriate care and monitoring are in place for affected patients. Depending on the findings, strategies may include lifestyle modifications, regular imaging follow-ups, or even surgical interventions if warranted.
Moreover, a structured plan includes ongoing assessments to adapt to any changes in the patient’s condition. This proactive approach is crucial, as it allows for timely interventions should complications arise.
12. Educating Patients and Families
Providing education on hepatic cystic lesions empowers patients and families to participate actively in care decisions. When patients understand their condition, they are more likely to engage in discussions about their health and follow recommended management strategies.
Additionally, consider creating resources or materials that explain what hepatic cystic lesions are, along with the potential next steps in management. Clear communication fosters trust and helps alleviate fears surrounding diagnosis and treatment.