Our Blog
Cystic Fibrosis and Its Role in Biliary Tree Complications
December 28, 2024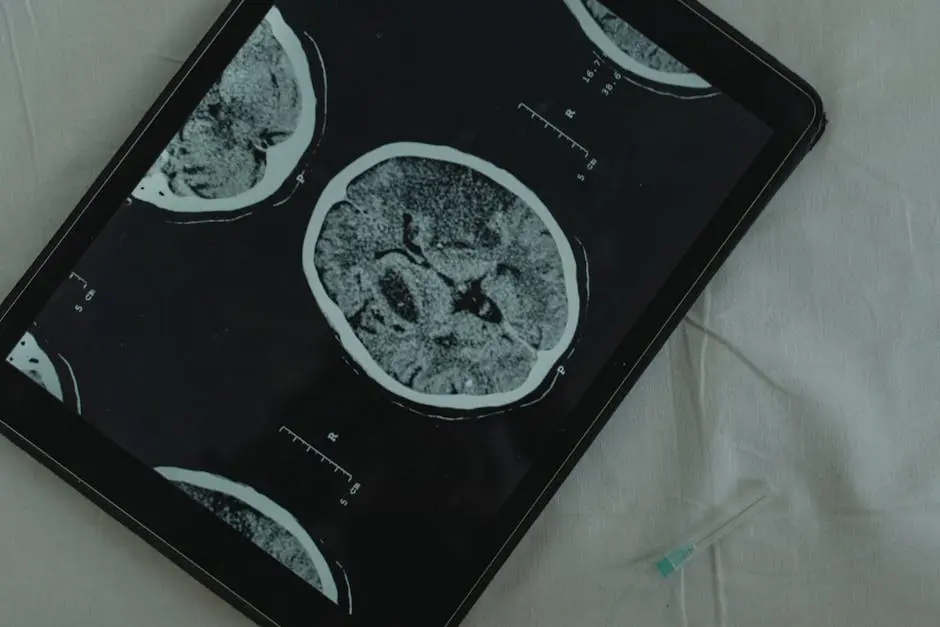
Cystic fibrosis (CF) is a genetic disorder that primarily affects the lungs and digestive system, but its implications can extend beyond these areas. One critical aspect to consider is its role in biliary tree complications. In this blog, we’ll explore how cystic fibrosis affects the biliary system, leading to complications, and we’ll learn what this means for patients and their care.
What is Cystic Fibrosis?
Cystic fibrosis is an inherited condition caused by mutations in the CFTR gene, affecting how salt and water move in and out of cells. This leads to thick, sticky mucus accumulation, particularly in the lungs and digestive tract. In this section, we will delve into the basic biology of CF and how it impacts the body.
Beyond the lungs, cystic fibrosis can have far-reaching effects. One fascinating aspect of this disorder is how the defective protein affects various organs, causing complications that might seem unrelated at first. For instance, the pancreas, which plays a crucial role in digestion, can become obstructed, leading to malabsorption and nutritional deficiencies. Consequently, patients often require supplemental enzymes to aid in digestion.
Moreover, the accumulation of thick mucus can create an environment conducive to infections, dramatically impacting a patient’s overall health. This points to the interconnectedness of bodily systems and how a genetic mutation can cascade into multiple health challenges. As we explore cystic fibrosis further, let’s keep in mind how these initial genetic changes can lead to broader complications.
Understanding the Biliary Tree
The biliary tree consists of a network of ducts that transport bile from the liver to the gallbladder and then to the small intestine. Bile is crucial for digestion, especially for fats. We’ll take a closer look at its function and structure in this section.
Bile is not just a digestive fluid—it’s a key player in our body’s ability to process nutrients. It aids in breaking down fats, making it easier for our bodies to absorb the vital nutrients we get from our food. If the biliary tree becomes compromised, as can happen with cystic fibrosis, it can disrupt this essential process.
Additionally, the biliary tree plays a role in the excretion of waste products from the liver. These functions are vital for metabolic health, and any hindrance could lead to severe complications. Understanding the nuances of this system helps us appreciate just how integral it is to maintaining overall health. A clearer view of the biliary tree also sets the stage for understanding how cystic fibrosis can pose challenges to its normal operation.
How Cystic Fibrosis Affects the Biliary System
Cystic fibrosis can lead to thickening of bile, resulting in blockages within the biliary tree. This can cause significant complications such as cholestasis, liver disease, and even infections. Here, we’ll discuss the mechanisms by which CF impacts the biliary system.
One of the most concerning effects of cystic fibrosis on the biliary system is cholestasis, which occurs when bile cannot flow from the liver to the duodenum. This buildup of bile can lead to liver complications, including fibrosis and cirrhosis over time. The pathophysiology behind this obstruction not only reveals the complexity of CF-related complications but also underscores the importance of early detection and intervention.
Furthermore, the interplay between thickened bile and biliary ducts can create a perfect storm for infection. As bile stagnates, it becomes a breeding ground for bacteria, which can lead to dangerous conditions like bacterial cholangitis. Thus, recognizing these factors is crucial for healthcare providers aiming to minimize risks for cystic fibrosis patients.
Common Biliary Complications in Cystic Fibrosis Patients
Patients with cystic fibrosis may experience various biliary complications, including gallstones, bile acid malabsorption, and biliary cirrhosis. This section will cover these issues in detail and their implications for patient health.
Gallstones are a common issue for those with cystic fibrosis due to the thickened bile. When bile becomes overly concentrated, crystals can form, leading to stones that may cause pain and further complications. Understanding the risk factors for gallstones is vital for proactive management.
Bile acid malabsorption, on the other hand, can lead to steatorrhea, a condition where fat is poorly absorbed, resulting in fatty stools. This can consequently lead to significant nutritional deficiencies. Patients may require dietary adjustments, emphasizing the importance of a tailored approach to their nutritional needs.
Finally, biliary cirrhosis represents a severe complication that requires prompt attention. Early signs might go unnoticed, yet as liver function deteriorates, significant health impacts can arise. Awareness of these complications is crucial for healthcare providers in navigating the care of cystic fibrosis patients effectively.
Management and Treatment Options for Biliary Complications
Effective management of biliary complications is key to improving outcomes for cystic fibrosis patients. We will explore the current treatment options, including medications, dietary changes, and potential surgical interventions.
Pharmacological treatments often focus on managing symptoms and preventing complications. For instance, ursodeoxycholic acid may help improve bile flow and reduce the concentration of bile, thereby alleviating some of the resulting issues.
Furthermore, dietary modifications play a crucial role in managing biliary-related issues. A high-fat diet is often encouraged in cystic fibrosis patients, but it must be tailored based on individual bile acid absorption capabilities. Nutritional interventions can be essential for maintaining health and vitality.
In some cases, surgical options may be necessary. Procedures such as bile duct exploration can relieve obstructions. When considering the best management strategies, a multidisciplinary approach involving nutritionists, gastroenterologists, and pulmonologists can yield the most beneficial outcomes for patients.
The Importance of Regular Monitoring
Regular monitoring of liver function and biliary health can help in the early detection of complications. In this section, we will discuss the importance of ongoing assessments and how they can lead to better patient care.
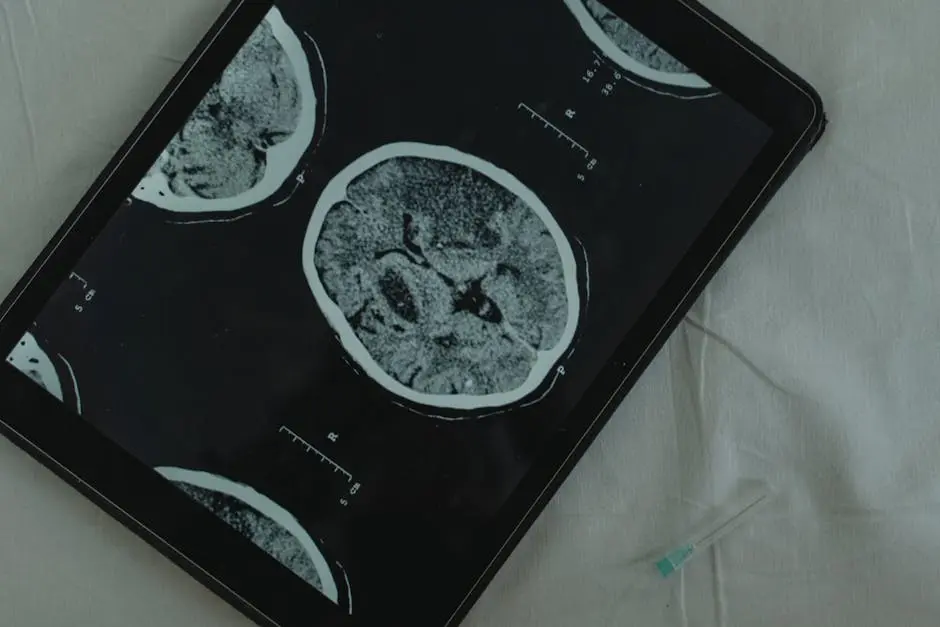
Monitoring liver enzymes and bilirubin levels, for example, can provide important insights into a patient’s biliary health. Regular ultrasound assessments of the biliary tree can help healthcare professionals identify blockages before they lead to more severe problems.
The impact of early detection cannot be overstated. By catching complications early, healthcare providers can initiate appropriate interventions sooner, potentially avoiding more drastic treatments later. In this way, a proactive approach not only preserves health but enhances overall well-being.
Wrapping Up: The Importance of Awareness in Cystic Fibrosis
Understanding the connection between cystic fibrosis and biliary tree complications is essential for effective management and care strategies. By addressing these complications proactively, caregivers and healthcare professionals can help improve the quality of life for individuals living with cystic fibrosis. Awareness and education can make a significant impact in navigating these challenges.